Mini-Percutaneous Nephrolithotomy Yields Higher Stone-Free Rate
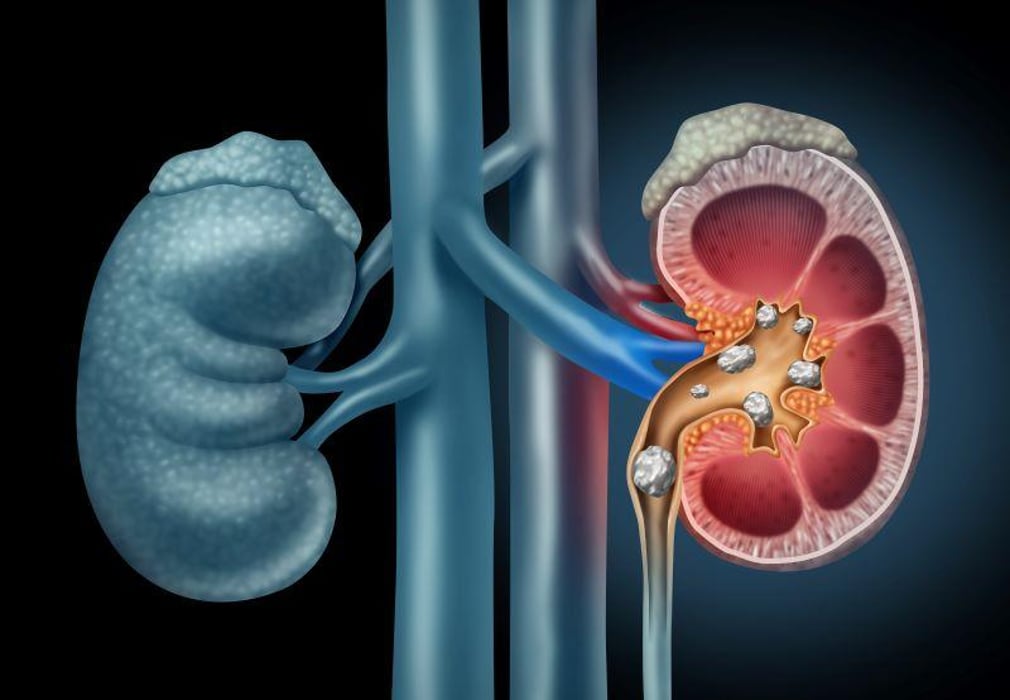
FRIDAY, May 26, 2023 (HealthDay News) -- Mini-percutaneous nephrolithotomy (mPCNL) is more likely to result in stone-free than flexible ureteroscopy for adults with renal stones of 1 to 2 cm in size, according to a study published in the June issue of The Journal of Urology.
Rahul Dutta, M.D., from Wake Forest University in Winston Salem, North Carolina, and colleagues evaluated the outcomes of ureteroscopy (50 patients) versus prone mPCNL (51 patients) for adults with 1-cm to 2-cm renal stones.
The researchers found that the stone-free rate was higher in the mPCNL group (76 versus 46 percent) when using a 2-mm cutoff. In the ureteroscopy group, the residual stone burden was significantly higher (3.6 versus 1.4 mm), whereas fluoroscopy time was significantly higher in the mPCNL group (273 versus 49 seconds). There were no significant differences noted in postoperative complications within 30 days, necessity of a secondary procedure within 30 days, or preoperative to postoperative creatinine change. Surgical time was also similar between the groups, but average length of stay was significantly higher in the mPCNL group. For mPCNL procedures, both net revenue and direct costs were higher, though they offset each other with a nonsignificant operating margin.
"In patients with intermediate-sized kidney stones, mini-PCNL may offer a more effective procedure, with similar safety and cost impact," senior author Jorge Gutierrez-Aceves, M.D., of the Cleveland Clinic, said in a statement.
Related Posts
Amid Shortages, Maker Says Restrictions on Wegovy Will Continue Into 2024
FRIDAY, Aug. 11, 2023 (HealthDay News) -- As demand for the wildly popular...
Federal Judge Overturns Texas Ban on School Mask Mandates
THURSDAY, Nov. 11, 2021 (HealthDay News ) -- A Texas ban on mask mandates in...
Another Study Links ‘Ultra-Processed’ Foods to Higher Cancer Risk
WEDNESDAY, Feb. 1, 2023 (HealthDay News) -- Fizzy sodas, microwaveable meals and...
Most Dog Breeds Are Highly Inbred — and Unhealthy
TUESDAY, Dec. 7, 2021 (HealthDay News) -- Traits particular to certain dog...
